Case Study
Matt is a 22-year-old Caucasian male, a resident of Dallas, Texas, who came to the emergency department
(ED) complaining of severe pain over his right chest area along with shortness of breath. He was injured
during a college football game. He stated that he was tackled from the front and the side by multiple
opponents. After the tackle, he was immediately short of breath and felt a sharp pain in the area of his right
chest. Matt was transferred by ambulance to a local hospital, with paramedics administering oxygen at 12
L/min via a non-rebreather mask. He also received a nebulized albuterol treatment. Along with oxygen
administration and breathing treatments, an 18-gauge IV catheter was placed in his left forearm. Upon
arrival at the hospital, the following medical history was gathered from the nurse. While obtaining the
medical history, the nurse took Matt’s vital signs and began a physical assessment.
Medical History
● Childhood-onset atopic asthma. – Uses two metered-dose inhalers (Symbicort and Serevent), twice
daily. Also uses an albuterol metered-dose inhaler when necessary.
● Previous diagnosis of moderate obstructive airway disease with marked bronchodilator response.
● His father died of an asthma exacerbation at age 50 a few years ago.
● All immunizations are up-to-date, albeit no tetanus shot.
● He has no smoking history, but does occasionally use marijuana brownies recreationally.
● Drinks alcohol a few times a month, usually during the weekend.
● He has no known drug allergies, but he avoids aspirin and aspirin-related medications.
● Other history was unremarkable.
Physical Assessment
Matt presents oriented to time, place, and location, but appears anxious and agitated. He also claims an
8/10 sharp right chest pain. Pupils are equal, round, and reactive to light and accommodation at 5 mm
bilaterally. His skin is pale with cyanosis noted around the lips despite the supplemental oxygen. The right
chest wall has scattered ecchymosis from his sternum to the axillary region. Auscultation of the lungs sound
diminished on the right with wheezing on the left side of his thorax. A murmur over his pulmonic valve is
noted. Palpation of the chest wall demonstrates subcutaneous emphysema on the right side of his neck
and tympanic hyperresonance with percussion over the right chest wall. Pulses are present in all four
extremities that are weak and rapid with a delayed capillary refill of three seconds.
1. A. What is likely the possible diagnosis?
B. Which symptoms and signs are related to that diagnosis?
2. While performing a physical assessment, a lab technician obtains blood samples from arterial and
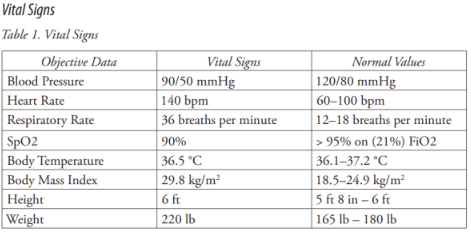
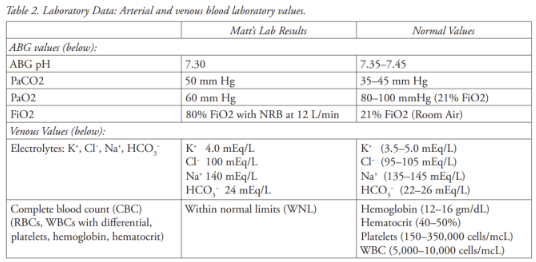
venous sources to be sent to the lab. Below is the result of laboratory analysis.
● EKG shows sinus tachycardia with left axis deviation and right ventricular strain pattern.
● Chest X-Ray notes hyperlucent right hemithorax, collapsed right lung, and the left tracheal
deviation as shown in the image below.
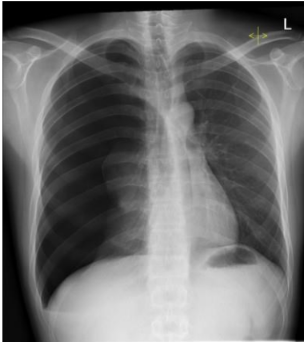
A. According to the paraclinical examination, can you confirm the patient’s diagnosis?
B. Give a proper definition of that diagnosis.
3. A. Interpret the ABGs for the injured football player
B. Explain the mechanism of how the tension pneumothorax caused the abnormal ABGs.
4. What is the routine treatment for a tension pneumothorax?
